Mitochondria, toxins, and supplements. What the labs say, not the internet.
Executive takeaways
Energy status predicts brain health because mitochondrial dysfunction disrupts synapses, metabolism, and circadian control before memory loss becomes obvious [ 1 , 2 , 3 ]. Modern cheek-swab assays make mitochondrial screening feasible without a biopsy, supporting earlier baselines and retesting [ 4 , 5 , 6 ]. Supplement megadosing, especially Vitamin D, raises preventable toxicity risks. Patients should dose only according to lab-monitored levels as directed by their Functional Physician, as Vitamin D requirements vary widely and change seasonally. Levels should be regularly monitored, as sunlight exposure, diet, and metabolism can significantly alter needs throughout the year.
Why does cellular energy predict brain health?
Answer: The brain’s extreme ATP demand makes mitochondria a leading indicator for cognition. In Alzheimer’s disease (AD), 2024–2025 reviews identify mitochondrial dysfunction as a central driver of pathogenesis, not a side effect [ 1 , 2 ]. Epidemiology underscores the scale: 7.2 million Americans ≥65 are living with AD in 2025, and 1 in 9 people ≥65 have AD dementia [ 16 ]. Circadian Biology, meaning proper sleep cycles, affects fundamental biological processes such as mitochondrial health, energy production, and biogenesis (the growth and division of mitochondria). Disruptions in sleep and circadian rhythm can therefore impair core biochemical functions, including energy production and detoxification (redox balance), ultimately impacting brain function and cognition.
Clinically useful information
- Screen energy first when patients report new fatigue, brain fog, or sleep fragmentation, even with normal memory testing.
- Pair cognitive screens with metabolic basics (fasting glucose variability, sleep efficiency, alcohol history) because these confound mitochondria-linked symptoms.
- Use question + metric pairs: “Is the patient waking refreshed?” + sleep efficiency ≥85%; “Is evening glycemia stable?” + post-prandial targets.

What changed in mitochondrial testing (and why it matters)?
Answer: You no longer need a muscle biopsy to ask mitochondrial questions. MitoSwab™ uses a buccal (cheek) swab to quantify respiratory-chain enzyme activity, enabling painless collection and practical retesting [ 4 , 6 ]. The provider discloses that performance characteristics were established in a CLIA-certified lab and that the test is not FDA-cleared or approved, important context for clinicians [ 5 ]. A comparative paper shows buccal enzyme analysis can mirror muscle biopsy patterns, supporting non-invasive screening alongside clinical judgment [ 6 ].
When to order
- Persistent fatigue + normal thyroid/iron → establish a mitochondrial baseline before trialing advanced therapies.
- Overtraining or post-illness slump → quantify enzyme activity, then retest 6–12 weeks after sleep, light, and protein interventions.
- Early cognitive complaints → combine cheek-swab data with sleep and glucose metrics to triage next steps.
How should we read NAD⁺/NADH, without the hype?
Answer: The NAD⁺/NADH ratio is a redox gauge that shapes calcium signaling, neurotransmission, and stress tolerance. A 2024 experiment raised the NAD⁺/NADH ratio using LbNOX/mitoLbNOX and recorded lower intracellular glutamate, smaller Ca²⁺ spikes, and reduced invasion in glioblastoma cells, direct evidence that shifting the ratio changes cell behavior [ 7 ]. A 2025 review details why simply “pushing NAD⁺ up” is not a free lunch; dosing must consider tissue context and downstream enzymes [ 8 ].
Measure twice, cut once; practical checklist
- Before NAD-pathway tactics: confirm sleep efficiency, late caffeine cut-off, alcohol frequency, and glycemic variability.
- Define success metrics up front (e.g., symptom scale, HRV trend, task performance) and retest in 6–8 weeks.
- Avoid stacking multiple NAD-boosting inputs simultaneously; change one variable per interval.
Are popular supplements helping or hurting - especially vitamin D?
Answer: Vitamin D helps when deficient and harms when overdosed. Patients should only supplement under the supervision of a Functional Physician and base their dose on individual lab-monitored levels rather than fixed amounts. Vitamin D should be regularly monitored, as levels can fluctuate significantly with seasonal changes, sunlight exposure, and individual metabolism. Proper adjustments prevent both deficiency and toxicity.
Social-media signal vs. clinical reality
- Analysis of 105 supplements promoted by influencers (2021–2023) found ingredient and claim patterns often inconsistent with evidence quality, highlighting risk of over-dosed products [ 11 ].
- Reviews of nutrition posts on Instagram report accuracy problems and widespread unsubstantiated claims, reinforcing a labs-first approach [ 12 ].
Two rules to prevent overshoot
- Test before you escalate: if 25(OH)D is already ≥40–50 ng/mL, reassess frequency and physician guidance.
- Retest every few months or sooner if symptoms suggest hypercalcemia (nausea, polyuria, confusion). Apply the same discipline to NAD⁺ boosters, berberine, and adaptogens: set target metrics and stop if no measurable benefit.
How do environmental toxicants drain ATP and amplify “wired-tired” fatigue?
Answer: 2024 toxicology reviews show metals and organic pollutants impair respiratory-chain complexes, raise ROS, and lower ATP output—a pattern that explains fatigue with paradoxical agitation [ 13 ]. Emerging 2025 reviews link nanoplastics to mitochondrial dysfunction across cell types through fission–fusion imbalance, membrane depolarization, and oxidative stress [ 14 ].
Low-cost sequence for patients
- Remove: use MERV-13 HVAC filters, switch to filtered water, and address workplace or hobby exposures.
- Bind: hit dietary fiber targets; consider binders only when exposure is verified and monitored.
- Rebuild: restore sleep/light rhythm and protein at 1.2–1.6 g/kg/day to support mitochondrial turnover.
What circadian and sleep levers measurably support brain energy?
Answer: Morning outdoor light, consistent sleep windows, and evening blue-light reduction improve redox balance and mitochondrial rhythms. Proper sleep cycles maintain mitochondrial health, energy production, and detoxification capacity. Disruption in these rhythms affects energy generation and cognition, underscoring that circadian hygiene is a biological foundation for brain health.
Four precise habits
- Get 10–20 minutes of outdoor light within 1 hour of waking.
- Keep sleep midpoint within a 1-hour band nightly.
- Stop caffeine after 2 p.m. to protect slow-wave sleep.
- Eat 1.2–1.6 g/kg/day protein, with 20–40 g at breakfast to stabilize daytime energy.
What is the “confounder cascade,” and why does order matter?
Answer: Complex problems respond to layered solutions. Address order first:
Sleep/light → glycemic control → protein adequacy → exposure reduction before adding mitochondria-targeted supplements. This sequence reduces noise in follow-up labs and clarifies cause-and-effect.
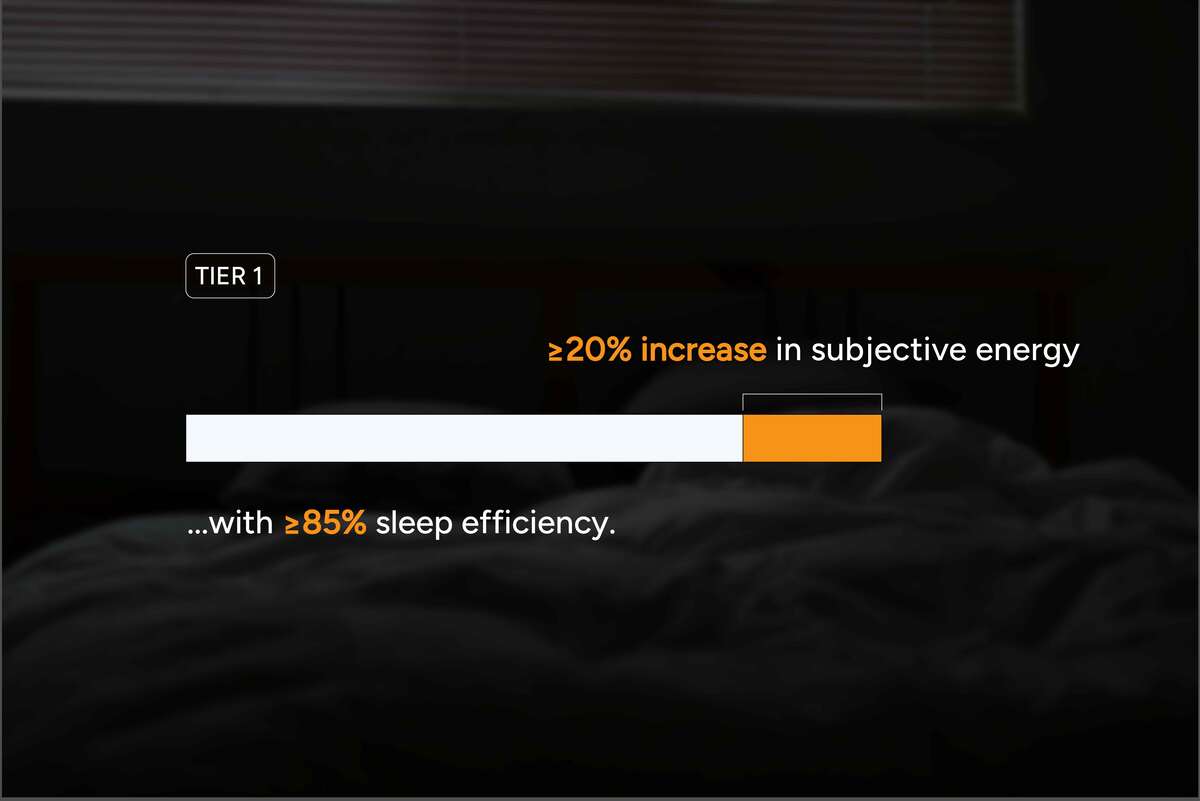
Tiered plan with checkpoints
- Tier 1 (weeks 0–4): circadian resets, caffeine cut-off, protein minimums; checkpoint = sleep efficiency ≥85% and subjective energy ↑ by ≥20%.
- Tier 2 (weeks 4–8): add targeted detox supports only if exposure is documented; checkpoint = reduction in symptom cluster by ≥30%.
- Tier 3 (week 8+): consider NAD-pathway tactics only with baseline labs and a retest date.
Methods & limits
We prioritized 2024–2025 peer-reviewed studies on mitochondria, circadian biology, toxicology, and supplementation. Non-FDA-cleared tests should be interpreted by qualified clinicians. Vitamin D and other nutrients must be managed under medical supervision using repeat labs to individualize care.
Works cited (not counted toward word length)
- Wei Y, et al. Mitochondrial transfer and dysfunction in Alzheimer’s disease. 2024. https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2024.1517965/full
- Kim J, et al. Circadian coordination: interplay between circadian clock and mitochondria. 2024. https://pmc.ncbi.nlm.nih.gov/articles/PMC11078072/
- Mir FA, et al. Unraveling the interplay between sleep, redox metabolism, and aging. 2025. https://pmc.ncbi.nlm.nih.gov/articles/PMC12133771/
- ReligenDx. MitoSwab™—Non-Invasive Mitochondrial Function Test. 2024. https://www.religendx.com/neurology/mitoswab-test/
- ReligenDx. Publications & test disclosures (CLIA; not FDA-cleared/approved). 2024. https://www.religendx.com/publications/
- Goldenthal MJ, et al. Non-invasive buccal enzyme dysfunction vs. muscle biopsy. 2012 (hosted 2024). https://www.religendx.com/wp-content/uploads/2024/06/non-invasive-evaluation-of-buccal-respiratory-chain-enzyme-dysfunction-in-mitochondrial-disease-comparison-with-studies-in-muscle-biopsyde.pdf
- Lee M, et al. Compartment-specific manipulation of NAD⁺/NADH by LbNOX/mitoLbNOX. Sci Rep, 2024. https://www.nature.com/articles/s41598-024-71462-8
- Yusri K, et al. The role of NAD⁺ metabolism and its modulation of mitochondria in aging and disease. 2025. https://www.nature.com/articles/s44324-025-00067-0
- NIH Office of Dietary Supplements. Vitamin D—Health Professional Fact Sheet. Updated June 27, 2025. https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/
- Yu C-H, et al. Over-supplement of vitamin D may cause delirium… Medicine (Baltimore), 2024. https://pmc.ncbi.nlm.nih.gov/articles/PMC11688089/
- Ricke JN, et al. Disinformation on dietary supplements by influencers on Instagram. Nutrients, 2024. https://pmc.ncbi.nlm.nih.gov/articles/PMC11985574/
- Denniss E, et al. Quality and accuracy of nutrition information on Instagram. Public Health Nutr, 2024. https://pmc.ncbi.nlm.nih.gov/articles/PMC10865719/
- Zuo M, et al. Mitochondrial Dysfunction in Environmental Toxicology. 2024. https://pubmed.ncbi.nlm.nih.gov/39485318/
- Liu H, et al. Environmental nanoplastics induce mitochondrial dysfunction (review). 2025. https://pubmed.ncbi.nlm.nih.gov/40550382/
- Microplastics and human cardiovascular risk (news summary). 2025. https://www.mrt.com/news/health_and_wellness/article/microplastics-artery-heart-risk-21053441.php
- 2025 Alzheimer’s Disease Facts & Figures. 2025. https://pmc.ncbi.nlm.nih.gov/articles/PMC12040760/
Related Resources

The Energy & Brain Health Report 2025
Mitochondria, toxins, and supplements. What the labs say, not the internet.
.jpg)
What Causes HPA Axis Dysfunction?
HPA axis dysfunction is primarily caused by chronic stress, affecting the normal interactions between your hypothalamus, pituitary gland, and adrenal glands. The Hypothalamic-Pituitary-Adrenal (HPA) axis plays a crucial role in your body's stress response, managing cortisol release and influencing overall health.

How Can I Get Tested for MTHFR?
You can get tested for MTHFR by requesting genetic testing from a healthcare provider who understands genetic mutations and their implications. MTHFR (methylenetetrahydrofolate reductase) mutations affect how the body processes folate and homocysteine, potentially impacting overall health significantly.
What Our have To Patients Say
FoundationMED always appreciates feedback from our valued patients. We’re thrilled to have an average rating of 5 out of 5 stars. Please read what others are saying about us below, and as always, we would love to collect your feedback.
LEARN MORE


